Smoking in 2026: A Persistent Public Health Threat
In 2026, smoking remains one of the most significant preventable causes of chronic disease in the United States. Although overall cigarette use has declined compared to previous decades, millions of adults continue to smoke. Dual use of traditional cigarettes and e-cigarettes is also increasingly common, adding complexity to modern tobacco dependence.
Public health data continue to confirm the serious health risks of smoking, including cardiovascular disease, chronic lung damage, and cancer. Despite widespread awareness, long-term cessation success remains difficult for many individuals. The challenge is not simply behavioral. Nicotine produces measurable neurochemical changes in the brain that reinforce dependence.
Modern clinical guidelines approach tobacco use as a chronic medical condition that benefits from structured treatment. Individuals seeking medically supervised support can learn more about prescription options such as Varenicline (Champix) for smoking cessation
In 2026, treatment strategies increasingly combine behavioral counseling with pharmacologic therapy to improve sustained abstinence rates. The goal is not only to encourage patients to quit, but to provide evidence-based support that addresses both withdrawal symptoms and long-term relapse prevention.
Smoking affects nearly every organ system. Damage accumulates silently over time, and many individuals feel relatively well until serious complications develop. Understanding the medical consequences of tobacco exposure often becomes the critical motivation for change.
Current research confirms that quitting smoking at any age improves health outcomes. Even long-term smokers experience measurable benefits after cessation. However, because nicotine alters dopamine pathways, unassisted quit attempts frequently result in relapse.
For this reason, physicians now emphasize comprehensive quit smoking medical treatment rather than relying solely on willpower. Before exploring therapeutic options, it is important to understand the major diseases directly caused by tobacco use.
Major Diseases Caused by Smoking
Smoking remains directly linked to some of the most serious chronic diseases in the United States. The biological mechanisms are well established and continue to be reinforced by long-term epidemiological studies.
Lung Disease and Chronic Respiratory Damage
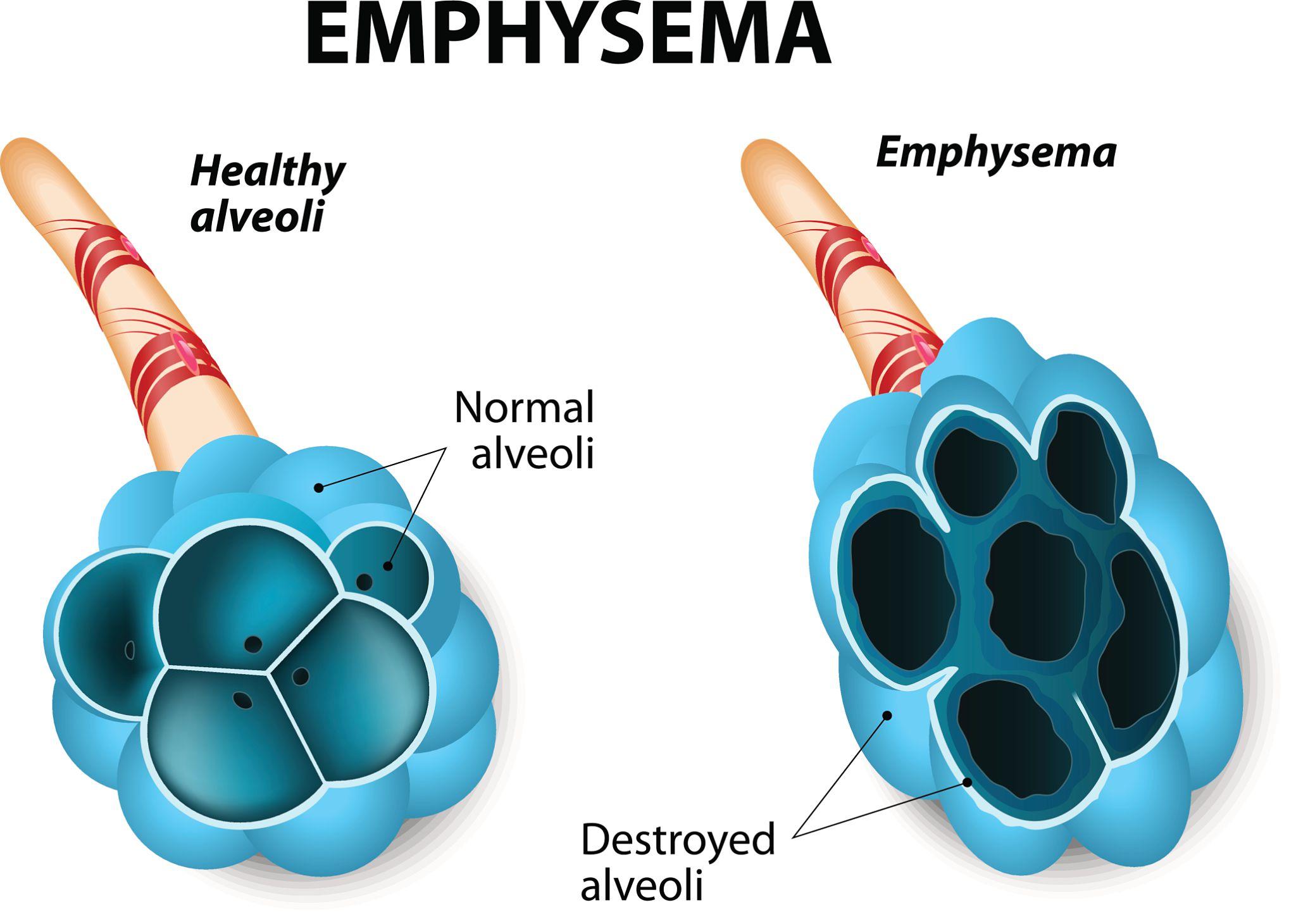
Chronic obstructive pulmonary disease, commonly known as COPD, includes emphysema and chronic bronchitis. It is one of the most common consequences of long-term tobacco use.
Tobacco smoke damages the alveoli, the small air sacs responsible for oxygen exchange. Over time, these structures lose elasticity and begin to break down. Inflammation thickens airway walls and increases mucus production. The result is progressive shortness of breath, chronic cough, and reduced oxygen delivery throughout the body.
Unlike many acute conditions, COPD is largely irreversible. While medications can reduce symptoms, they cannot fully restore destroyed lung tissue. The only proven intervention that slows disease progression is smoking cessation.
Clinical data show that individuals who stop smoking experience stabilization in lung function decline. Although lost capacity cannot be fully regained, quitting prevents further structural destruction.
Cardiovascular Disease
Smoking significantly increases the risk of heart attack, stroke, and peripheral artery disease. Nicotine raises blood pressure and heart rate, while carbon monoxide reduces oxygen availability in the bloodstream.
More importantly, tobacco toxins damage the endothelial lining of blood vessels. This promotes inflammation and accelerates atherosclerosis, the buildup of plaque inside arteries. Narrowed arteries restrict blood flow and increase the likelihood of clot formation.
In 2026, cardiology research continues to demonstrate that smokers face substantially higher rates of myocardial infarction compared to non-smokers. Even younger adults who smoke show early signs of vascular dysfunction.
Encouragingly, cardiovascular risk decreases relatively quickly after cessation. Within one year of quitting, the risk of coronary heart disease drops significantly compared to continued smoking.
Cancer and Genetic Damage
Smoking is the leading cause of lung cancer and is strongly associated with cancers of the throat, esophagus, pancreas, kidney, and bladder.
Tobacco smoke contains thousands of chemical compounds, including multiple known carcinogens. These substances directly damage DNA and impair cellular repair mechanisms. Over time, repeated genetic mutations increase the likelihood of malignant transformation.
Cancer risk is influenced by both duration and intensity of exposure. However, quitting smoking reduces cumulative risk. Former smokers experience a gradual decline in cancer incidence compared to those who continue smoking.
Prevention remains the most effective oncology strategy. Eliminating tobacco exposure is one of the most impactful steps an individual can take to reduce long-term cancer risk.
Neurological and Mental Health Effects
Nicotine alters dopamine signaling in the brain, reinforcing repeated use and creating dependency. While smokers may experience short-term stimulation or stress relief, long-term use is associated with increased baseline anxiety and mood instability.
Withdrawal symptoms often include irritability, restlessness, sleep disturbance, and difficulty concentrating. These symptoms contribute to relapse when individuals attempt to quit without medical support.
Understanding nicotine dependence as a biological condition rather than a behavioral weakness is essential in 2026. This shift has changed how healthcare providers approach smoking cessation therapy.
Key Health Consequences of Smoking
The cumulative effects of tobacco use include:
- Progressive and irreversible lung damage
- Increased risk of heart attack and stroke
- Higher incidence of multiple cancers
- Accelerated vascular aging
- Persistent nicotine dependence
These consequences highlight why early intervention matters. The longer smoking continues, the greater the structural and genetic damage.
The encouraging reality is that cessation changes the trajectory of disease risk. Lung function decline slows, cardiovascular risk decreases, and long-term cancer probability gradually drops. However, because nicotine creates physiological dependence, most individuals benefit from structured medical treatment rather than attempting to quit alone.
Why Nicotine Addiction Is So Difficult to Overcome
Nicotine dependence is not simply a habit. It is a biologically driven condition that alters brain chemistry and reinforces repeated exposure. When nicotine enters the bloodstream, it rapidly crosses the blood-brain barrier and binds to nicotinic acetylcholine receptors, particularly the alpha4beta2 subtype.
Activation of these receptors triggers dopamine release in the brain’s reward pathway. Dopamine reinforces behavior, creating a cycle of craving and temporary relief. Over time, the brain adapts to repeated stimulation. Tolerance develops, and individuals require continued nicotine intake to maintain normal dopamine levels.
When smoking stops, dopamine levels drop. This produces withdrawal symptoms that can begin within hours. These symptoms often peak during the first week but may persist for several weeks.
Common nicotine withdrawal symptoms include:
- Irritability and mood changes
- Anxiety or restlessness
- Difficulty concentrating
- Sleep disturbance
- Increased appetite
Because these symptoms are uncomfortable, many individuals relapse even when they strongly intend to quit. This explains why unassisted quit attempts frequently fail despite high motivation.
In 2026, medical guidelines recognize tobacco use disorder as a chronic relapsing condition. As with other chronic diseases, treatment improves outcomes. This understanding has shifted the focus toward evidence-based smoking cessation treatment rather than relying on willpower alone.
ИНФОГРАФИКА
Evidence-Based Smoking Cessation Options in 2026
Modern clinical practice supports a combination of pharmacologic therapy and behavioral counseling. Multiple therapeutic options are available, but effectiveness varies.Nicotine replacement therapy provides controlled doses of nicotine through patches, gum, lozenges, inhalers, or nasal sprays. These products reduce withdrawal intensity but do not directly block nicotine reward from cigarettes.
Bupropion, an antidepressant medication, reduces cravings by influencing norepinephrine and dopamine pathways. It can be effective, particularly for individuals with coexisting depressive symptoms.Varenicline, originally marketed as Champix, works differently. It acts as a partial agonist at nicotinic receptors. This means it partially stimulates the receptor to reduce withdrawal while simultaneously blocking nicotine from fully activating it if a person smokes.
Comparative research continues to demonstrate higher sustained abstinence rates with varenicline compared to single-form nicotine replacement therapy. Combination approaches may further improve outcomes for selected patients.
The table below summarizes current data from long-term cessation studies.
| Treatment | 6-Month Abstinence Rate | Prescription Required | Common Side Effects |
|---|---|---|---|
| Nicotine Replacement Therapy | 15 to 20 percent | No | Skin irritation, insomnia |
| Bupropion | 18 to 25 percent | Yes | Dry mouth, insomnia |
| Varenicline | 25 to 35 percent | Yes | Nausea, vivid dreams |
| Behavioral Therapy Alone | 10 to 15 percent | No | None |
While no treatment guarantees success, medications significantly improve the likelihood of sustained abstinence compared to behavioral counseling alone.
Importantly, treatment selection should consider:
- Medical history
- Psychiatric history
- Renal function
- Prior quit attempts
- Patient preference
Personalized therapy is central to modern quit smoking medical treatment strategies.
How Varenicline Works in Smoking Cessation
Varenicline remains one of the most studied and widely used prescription medications for tobacco cessation in 2026. Its mechanism addresses both the biological and behavioral aspects of nicotine addiction.
As a partial agonist at alpha4beta2 nicotinic receptors, varenicline produces moderate receptor stimulation. This helps reduce cravings and withdrawal symptoms. At the same time, if a person smokes while taking varenicline, nicotine cannot fully activate the receptor. This reduces the rewarding sensation associated with cigarettes.
This dual mechanism provides two advantages:
- Reduced intensity of withdrawal symptoms
- Decreased satisfaction from smoking
Clinical trials consistently show improved long-term abstinence rates when varenicline is used as directed for a standard 12-week course. Some patients benefit from extended therapy to reduce relapse risk.
For a detailed review of clinical outcomes and updated research findings, see the in-depth analysis in Varenicline effectiveness and safety overview
In addition to pharmacologic effects, varenicline is most effective when combined with structured behavioral support. Counseling, follow-up visits, and digital health programs increase adherence and reinforce coping strategies.
The broader clinical context of how this medication fits into comprehensive tobacco cessation plans is explored in The role of Champix in smoking cessation/
By 2026, treatment models increasingly integrate telehealth consultations and remote monitoring. This allows physicians to adjust dosing, manage side effects, and support adherence without requiring frequent in-person visits.
Varenicline requires a prescription in the United States. A healthcare provider evaluates medical history, discusses potential side effects, and determines whether the medication is appropriate.
Safety Considerations and What to Discuss With Your Doctor
As with any prescription medication, varenicline (Champix) for smoking cessation requires medical evaluation before initiation. While it is considered effective and generally well tolerated, individual risk factors must be assessed. The most commonly reported side effect is nausea, which is usually mild to moderate and often improves over time. Taking the medication after food and with a full glass of water may help reduce gastrointestinal discomfort. Some patients report sleep changes, including vivid dreams or insomnia. These effects are typically manageable but should be discussed during follow-up visits.
Large post-marketing studies have not confirmed a significant increase in severe psychiatric events in the general population. However, individuals with a history of depression, anxiety disorders, or other psychiatric conditions should be monitored appropriately during treatment. Kidney function should also be reviewed before starting therapy, as dosing adjustments may be necessary in cases of renal impairment.
Before prescribing quit smoking medication, healthcare providers typically evaluate:
- Past quit attempts and response to previous therapies
- Current medications and potential drug interactions
- Mental health history
- Kidney function
- Level of nicotine dependence
Open communication between patient and physician improves both safety and treatment success. Follow-up visits allow dose adjustments, management of side effects, and reinforcement of behavioral strategies.
How Varenicline (Champix) Targets Nicotine Dependence
Nicotine binds to specific receptors in the brain, stimulating dopamine release and reinforcing repeated smoking behavior. When nicotine intake stops, receptor stimulation drops, leading to withdrawal symptoms and cravings.
Champix (Varenicline) partially stimulates these same receptors while blocking nicotine from fully activating them. This dual mechanism helps reduce craving intensity and decreases the rewarding effect of cigarettes if smoking occurs during treatment.
By addressing both withdrawal and reward pathways, evidence-based smoking cessation treatment becomes more biologically targeted rather than purely behavioral.
Why 2026 Is the Right Time to Quit
The medical evidence is clear. Smoking contributes to chronic lung disease, cardiovascular events, cancer, and long-term neurological dependence. Damage accumulates over time, but cessation alters the trajectory of risk. In 2026, quitting smoking is supported by advanced treatment strategies, improved clinical data, and expanded telehealth access. Structured therapy significantly increases long-term success compared to unassisted attempts. Prescription medications such as varenicline provide a mechanism-based approach to nicotine dependence. When combined with behavioral counseling and medical supervision, they improve sustained abstinence rates.
For individuals ready to stop smoking, seeking professional guidance is an important first step toward reducing long-term disease risk and improving overall health.
Medical Disclaimer
This article is for informational purposes only and does not constitute medical advice. Always consult a qualified healthcare professional regarding any medical condition or treatment.
Author:
Dr. Cody R. Christensen
FAQ: Most Common Questions About Quitting Smoking and Varenicline
Is varenicline more effective than nicotine patches?
Clinical studies show higher long-term abstinence rates with varenicline compared to single-form nicotine replacement therapy. Treatment choice should be individualized based on medical history and patient preference.
How long does varenicline treatment usually last?
The standard course is 12 weeks, though some patients may benefit from extended therapy to reduce relapse risk. A healthcare provider determines the appropriate duration.
Are there serious psychiatric risks associated with varenicline?
Large studies have not shown a significant increase in severe psychiatric events in the general population. Patients with prior mental health conditions should be monitored during treatment.
Can varenicline help people who use both cigarettes and e-cigarettes?
Emerging evidence suggests it may support cessation in dual users by reducing nicotine cravings. Individual evaluation is recommended to determine the most appropriate strategy.
Do I need a prescription to start varenicline in the United States?
Yes, varenicline requires a prescription from a licensed healthcare provider. A medical consultation ensures appropriate dosing and monitoring.
