Why Autoimmune and Parasitic Diseases Still Matter in 2026
Overview
In 2026, both chronic autoimmune disorders and infectious diseases remain significant contributors to global morbidity. While medical innovation has improved diagnostics and therapeutic precision, many inflammatory and parasitic conditions still require long-term pharmacologic management.
Autoimmune diseases such as lupus and rheumatoid arthritis continue to rise in prevalence. At the same time, international travel and global migration patterns sustain the clinical relevance of parasitic infections, including malaria. These two categories of disease may appear unrelated, yet they share a common therapeutic history through the use of medications such as chloroquine.
Originally developed as an antimalarial agent, chloroquine has been used for decades in infectious disease treatment. Over time, researchers identified additional immunomodulatory properties, expanding its application to selected autoimmune conditions. Today, understanding chloroquine uses requires looking at both infectious and inflammatory contexts.
For patients and clinicians seeking detailed information about formulation, prescribing, and clinical context, more information is available on the dedicated page for Aralen medication (chloroquine)
Modern treatment strategies emphasize individualized therapy. Not every patient with an autoimmune disease or parasitic infection is a candidate for the same medication. Risk factors, comorbidities, and safety considerations must guide decision-making. In 2026, the focus has shifted toward balancing therapeutic benefit with long-term monitoring.
Before exploring how chloroquine functions within current treatment plans, it is important to understand the diseases in which it has historically played a role.
Parasitic Infections: Malaria and Ongoing Global Risk
Malaria remains one of the most studied parasitic infections worldwide. Although the United States does not experience endemic transmission, imported cases continue to occur each year due to international travel. In regions where chloroquine-sensitive strains of Plasmodium remain present, chloroquine treatment guidelines still recognize its therapeutic value.
Malaria is caused by Plasmodium parasites transmitted through the bite of infected Anopheles mosquitoes. Once inside the bloodstream, parasites invade red blood cells, multiply, and trigger systemic symptoms.
Common malaria symptoms include:
- Fever
- Chills
- Headache
- Muscle pain
- Fatigue
If untreated, malaria can progress to severe complications, including anemia, organ dysfunction, and cerebral involvement. Early diagnosis and appropriate pharmacologic treatment are essential to prevent complications.
Historically, chloroquine was one of the most widely used antimalarial medications. Its mechanism involves interfering with parasite growth inside red blood cells. However, the emergence of drug-resistant strains has reduced its effectiveness in some regions. For this reason, current malaria treatment protocols vary depending on geographic resistance patterns.
Despite these limitations, FDA approved uses of chloroquine continue to include treatment of malaria caused by susceptible strains. In selected settings, chloroquine remains part of recommended therapeutic regimens.
Understanding the infectious disease context clarifies one important dimension of chloroquine uses. However, infectious disease treatment represents only part of its clinical relevance.
Expanding Beyond Infection: The Autoimmune Connection
The discovery that chloroquine has immunomodulatory properties significantly expanded its therapeutic profile. Researchers observed that beyond its antiparasitic effects, the medication could influence immune signaling pathways involved in chronic inflammation.
This observation led to its use in certain autoimmune diseases, particularly systemic lupus erythematosus and rheumatoid arthritis. In these conditions, the immune system mistakenly targets healthy tissues, leading to persistent inflammation and organ damage.
Autoimmune Diseases and Chronic Inflammation
Autoimmune diseases develop when the immune system mistakenly attacks healthy tissues. Instead of distinguishing between foreign pathogens and the body’s own cells, immune responses become misdirected. This results in chronic inflammation that can affect joints, skin, kidneys, blood vessels, and other organs.
In 2026, autoimmune disorders remain a significant clinical burden in the United States. Conditions such as systemic lupus erythematosus and rheumatoid arthritis often require long-term management. These diseases are characterized by periods of flare and remission, making consistent monitoring and tailored therapy essential.
Chronic inflammation is driven by immune cell activation and signaling molecules that perpetuate tissue damage. Without treatment, inflammation may lead to irreversible structural changes. For example, untreated rheumatoid arthritis can result in joint destruction, while lupus may affect kidney function or cardiovascular health.
This is where medications with immunomodulatory properties become clinically relevant. Beyond its traditional infectious disease applications, chloroquine for autoimmune disease has been used in selected patients to help regulate immune overactivity.
The immunologic effects of chloroquine include modulation of antigen presentation and interference with intracellular signaling pathways that contribute to inflammation. These properties make it useful in certain inflammatory disorders when prescribed under appropriate supervision.
In modern autoimmune disease treatment, therapy is rarely limited to a single medication. Physicians often combine agents depending on disease severity and organ involvement. Chloroquine may be considered as part of a broader therapeutic strategy rather than as standalone therapy.
Key goals of autoimmune treatment include:
- Reducing inflammatory activity
- Preventing long-term organ damage
- Minimizing flare frequency
- Maintaining quality of life
In 2026, individualized therapy remains central. Treatment decisions depend on disease severity, comorbidities, laboratory findings, and patient tolerance. Not all autoimmune patients are candidates for the same medications, which is why understanding the mechanism of action is important.
How Chloroquine Works in the Body
To understand chloroquine uses, it is helpful to examine its mechanism of action in both parasitic and autoimmune contexts.
In malaria, chloroquine accumulates within the parasite’s digestive vacuole. It interferes with the parasite’s ability to detoxify heme, a byproduct of hemoglobin digestion. The buildup of toxic compounds ultimately damages the parasite and leads to its destruction.
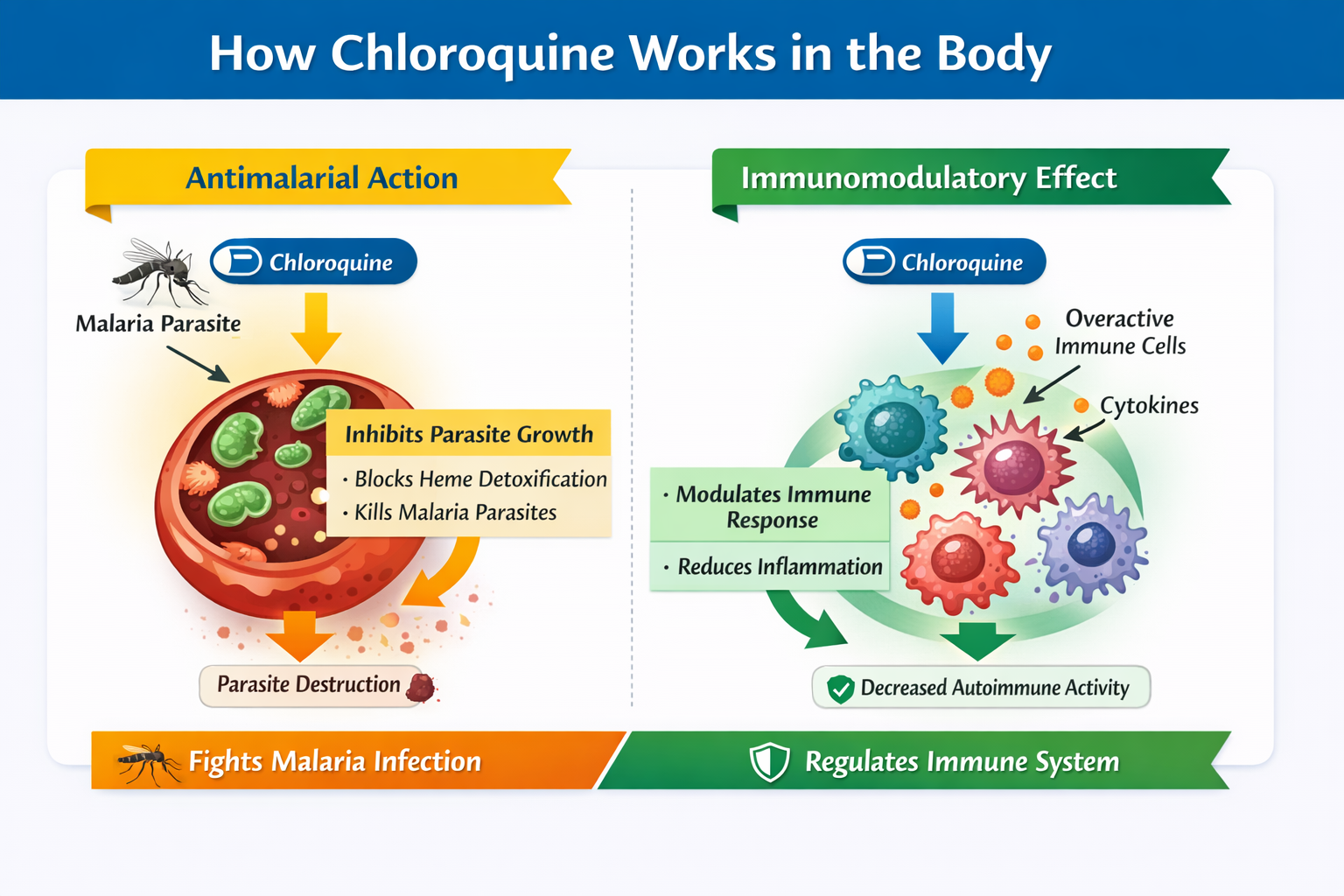
In autoimmune diseases, the mechanism is different but equally significant. Chloroquine affects immune cell signaling pathways. It increases the pH within intracellular compartments, altering antigen processing and reducing activation of certain immune receptors. This leads to decreased inflammatory signaling.
Through these effects, chloroquine can moderate immune responses that drive chronic inflammation. However, its immunomodulatory impact is not as broad as that of some newer biologic agents. For this reason, its use in 2026 is typically selective and guided by specific clinical scenarios.
Importantly, the benefits of treatment must always be weighed against potential risks. While discussing therapeutic mechanisms, clinicians also evaluate the overall Aralen safety profile.
Before initiating therapy, physicians assess:
- Baseline eye health due to potential retinal toxicity
- Cardiac history, particularly rhythm abnormalities
- Liver and kidney function
- Concurrent medications that may interact
These precautions are part of responsible prescribing practices. Long-term therapy may require periodic monitoring, especially when used for chronic autoimmune conditions. Another area frequently discussed in clinical practice involves comparisons between related medications. Patients often ask about differences between chloroquine and hydroxychloroquine, particularly regarding safety and effectiveness.
Chloroquine vs Hydroxychloroquine: Clinical Differences in 2026
Patients and clinicians frequently compare chloroquine vs hydroxychloroquine, especially in the context of autoimmune management. While both medications share structural similarities and historical antimalarial origins, they are not identical in pharmacologic profile or safety considerations.
Hydroxychloroquine was developed as a derivative of chloroquine with the goal of improving tolerability. Over time, it became more commonly prescribed in autoimmune conditions due to a comparatively lower risk of certain adverse effects, particularly retinal toxicity at standard doses.
Chloroquine, marketed as Aralen medication, remains FDA-approved for specific indications, particularly malaria caused by susceptible strains. Its use in autoimmune conditions is more selective in 2026 and typically guided by clinical judgment and patient-specific factors.
Below is a comparative overview.
| Feature | Chloroquine (Aralen) | Hydroxychloroquine |
|---|---|---|
| Primary FDA-approved use | Malaria treatment | Malaria treatment |
| Autoimmune use | Selected lupus and inflammatory cases | More commonly used in lupus and rheumatoid arthritis |
| Retinal toxicity risk | Higher with long-term exposure | Lower but still requires monitoring |
| Monitoring requirements | Regular ophthalmologic exams | Regular ophthalmologic exams |
| Current clinical preference | Used selectively | More frequently prescribed for autoimmune disease |
While hydroxychloroquine is more commonly used for chronic inflammatory conditions, chloroquine may still be considered depending on availability, patient response, and physician assessment.
Understanding these distinctions is important when evaluating overall chloroquine treatment 2026 strategies.
Safety Profile and Monitoring in 2026
Any discussion of chloroquine uses must include a careful review of safety considerations. The Aralen safety profile is well documented through decades of clinical experience, but appropriate monitoring remains essential.
Common adverse effects may include gastrointestinal discomfort, headache, and mild visual disturbances. More serious concerns, although less common, involve retinal toxicity and cardiac rhythm abnormalities, particularly with prolonged use or high cumulative doses.
Because of these risks, structured monitoring protocols are recommended during long-term therapy.
Before initiating treatment, physicians typically evaluate:
- Baseline ophthalmologic status
- Cardiac history, including arrhythmia risk
- Liver and kidney function
- Potential drug interactions
Periodic eye examinations are particularly important in chronic autoimmune therapy. Retinal changes may develop gradually and can be asymptomatic in early stages. Early detection helps prevent permanent visual impairment. Cardiac monitoring may also be considered in patients with known risk factors. In 2026, clinicians increasingly use individualized risk assessment rather than uniform protocols for all patients.
It is important to emphasize that no medication is universally appropriate. Decisions regarding autoimmune disease treatment or malaria management depend on diagnosis, disease severity, and patient-specific health factors.
The Role of Aralen in Modern Treatment Plans
In contemporary practice, Aralen medication is not viewed as a one-size-fits-all therapy. Instead, it is considered one option within a broader therapeutic framework.
For malaria caused by chloroquine-sensitive strains, it remains a recognized treatment. In autoimmune conditions, it may be selected in specific cases when benefits outweigh potential risks.
Modern treatment planning in 2026 emphasizes:
- Evidence-based prescribing
- Individualized dosing
- Ongoing monitoring
- Shared decision-making between physician and patient
Understanding the context of chloroquine (aralen) for autoimmune disease and infectious indications helps patients make informed decisions in collaboration with healthcare providers.
Medical Disclaimer
This article is for informational purposes only and does not constitute medical advice. Always consult a qualified healthcare professional regarding any medical condition or treatment.
Author:
Dr. Cody R. Christensen
F.A.Q
What is chloroquine used for in 2026?
Chloroquine is primarily used for malaria caused by susceptible strains and in selected autoimmune conditions. Its use depends on geographic resistance patterns and individual patient factors.
Is Aralen still prescribed for malaria?
Yes, Aralen is prescribed for malaria in regions where parasites remain sensitive to chloroquine. Treatment choice depends on resistance data and clinical guidelines.
What are the main chloroquine side effects?
Common side effects include gastrointestinal discomfort and headache. Long-term use may require monitoring for retinal or cardiac complications.
How is chloroquine different from hydroxychloroquine?
Hydroxychloroquine is structurally related but generally associated with a lower risk of certain adverse effects. Both medications require medical supervision.
Do patients need monitoring while taking Aralen?
Yes, regular medical evaluation is recommended, especially for long-term therapy. Monitoring helps detect potential eye or cardiac complications early.
Sources
- FDA – Official safety information noting approved uses of chloroquine and hydroxychloroquine, including for malaria and autoimmune conditions.
- NIH/NCBI – Clinical overview of chloroquine, including indications, mechanism of action, adverse effect profile, and monitoring considerations.
- CDC Yellow Book – Guidance on malaria treatment and prophylaxis relevant to chloroquine-sensitive regions and side effect considerations.
- Wikipedia – General, well-cited overview of chloroquine’s pharmacology, history, indications, and safety considerations.
