What Is Female Erectile Dysfunction
Definition and Overview
Female erectile dysfunction is a physiological condition in which a woman has difficulty achieving or maintaining adequate genital arousal during sexual activity. Although the term erectile dysfunction is widely associated with men, women also have erectile tissue, primarily within the clitoris and surrounding structures. This tissue relies on healthy blood circulation, intact nerve pathways, and balanced hormones.
When any part of this system is disrupted, physical arousal may become weaker, slower, or inconsistent. A woman may notice reduced clitoral swelling, insufficient lubrication, decreased sensitivity, or difficulty sustaining physical excitement. These changes can occur at any age, though risk increases with hormonal shifts, chronic illness, or certain medications.
In clinical practice, this condition is often categorized as Female Sexual Arousal Disorder. However, the term female erectile dysfunction emphasizes the vascular component of the issue. Just like male erectile function, female genital response depends on proper blood vessel dilation and nitric oxide activity.
How Female Arousal Works
Female arousal begins with mental stimulation. Emotional connection, physical touch, visual cues, or erotic thoughts activate brain centers responsible for pleasure and motivation. These signals travel through the spinal cord and stimulate nerves connected to genital tissues.
Blood vessels in the clitoris and vaginal walls dilate, allowing increased circulation. The clitoris becomes engorged with blood, sensitivity rises, and lubrication develops. Estrogen maintains tissue health and elasticity, while androgens contribute to sensory responsiveness.
If vascular dilation is limited, clitoral engorgement may be incomplete. If nerve communication is weakened, sensitivity can decline. If hormonal balance shifts significantly, lubrication and comfort may be affected. Female erectile dysfunction typically reflects impairment at one or more points in this coordinated process.
Female Erectile Dysfunction Versus Low Libido
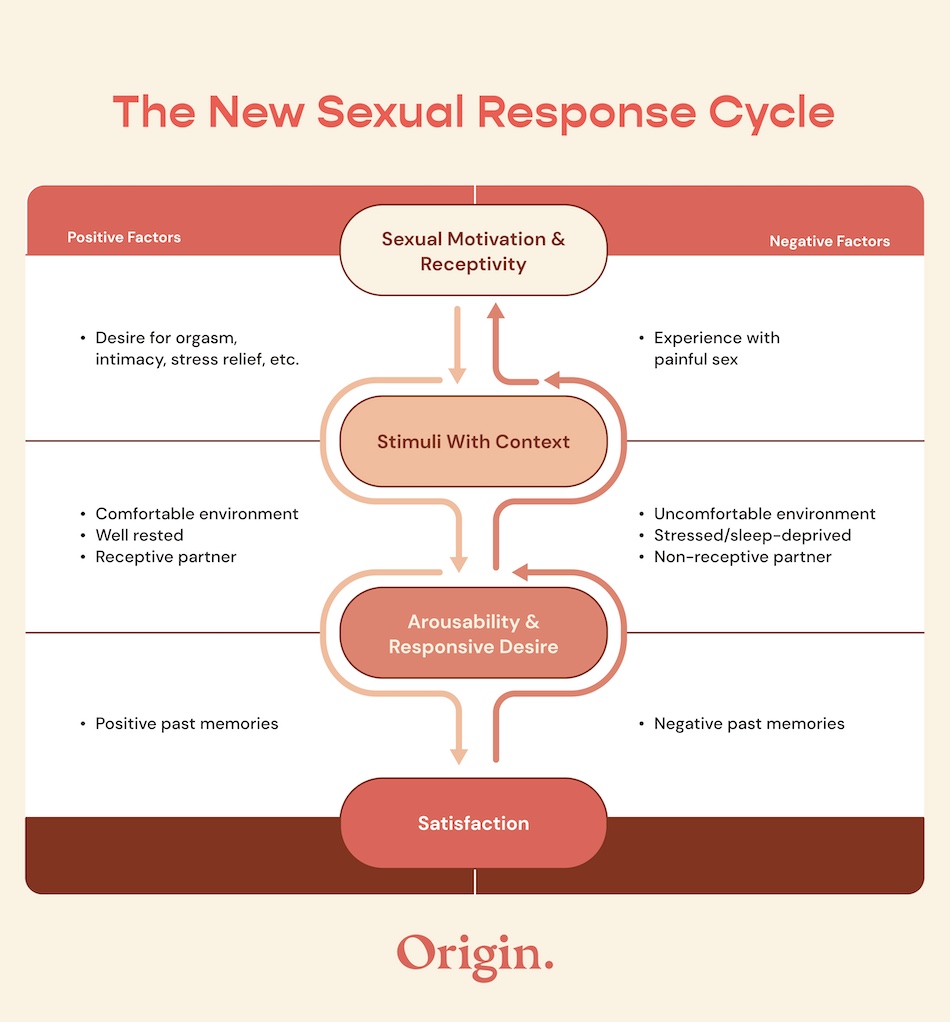
It is important to distinguish female erectile dysfunction from low libido. Libido refers to sexual desire, meaning psychological interest in intimacy. Erectile dysfunction refers to difficulty with the physical response of the body.
A woman may feel desire yet experience weak lubrication or reduced clitoral sensitivity. Conversely, she may have normal physical responsiveness but little interest in sex. Because these mechanisms are different, identifying which system is affected is essential for choosing the correct treatment strategy.
Early Signs and Warning Indicators
Early symptoms are often subtle. Many women assume changes in arousal are temporary or stress related. However, persistent physical changes may indicate an underlying medical issue.
Common warning signs include difficulty becoming physically aroused despite adequate stimulation, reduced genital sensitivity, insufficient lubrication, weaker clitoral swelling, and decreased sexual satisfaction directly linked to physical response.
Occasional variability is normal. When symptoms persist for several months and cause distress, medical evaluation is recommended.
Causes and Risk Factors of Female Erectile Dysfunction
Female erectile dysfunction develops when one or more components of the sexual response system fail to function optimally. Because female arousal is a coordinated neurovascular and hormonal process, disruption can occur at multiple levels simultaneously. Understanding the cause is critical for selecting the right treatment rather than masking symptoms.
Hormonal Shifts
Hormonal fluctuation is one of the most common triggers of persistent arousal problems. Estrogen maintains vaginal elasticity, supports lubrication, and helps regulate blood vessel responsiveness. Testosterone, although present in lower levels in women, contributes to genital sensitivity and overall responsiveness to stimulation. During perimenopause and menopause, declining estrogen levels often result in vaginal dryness and reduced tissue flexibility. Postpartum hormonal changes, thyroid dysfunction, elevated prolactin, and certain hormonal contraceptives may also affect arousal. When hormonal balance shifts significantly, the physical phase of sexual response can weaken even if desire remains present.
Vascular Impairment
Genital engorgement depends on adequate blood flow. Conditions that impair endothelial function reduce the ability of blood vessels to dilate properly. Cardiovascular disease, hypertension, high cholesterol, insulin resistance, and diabetes can all affect vascular health.
Because the clitoris contains erectile tissue that requires increased circulation during stimulation, even mild vascular dysfunction may lead to weaker swelling or delayed arousal. Smoking further restricts blood flow and reduces nitric oxide availability, directly impacting genital response.
Neurological Factors
Arousal requires intact communication between the brain and genital nerves. Neurological disorders such as multiple sclerosis, spinal cord injury, or diabetic neuropathy can interfere with this signaling. Even without diagnosed neurological disease, chronic stress alters neural pathways over time and may blunt responsiveness.
Psychological stress increases cortisol, which can suppress sexual signaling. When stress becomes persistent, the brain prioritizes survival pathways rather than pleasure pathways, reducing the intensity of arousal.
Medication Effects
Several commonly prescribed medications are associated with reduced sexual responsiveness. Selective serotonin reuptake inhibitors may blunt arousal and delay orgasm. Some antihypertensive drugs, antihistamines, and hormonal treatments can decrease lubrication or sensitivity.
If symptoms begin after initiating a new prescription, medication review is essential. Adjustments may restore normal response without requiring additional treatment.
Psychological and Relationship Influences
Emotional well being significantly influences physical arousal. Depression, anxiety, past trauma, body image concerns, and unresolved relationship conflict may inhibit sexual response even when vascular function is intact.
Physical and psychological factors often reinforce each other, creating a cycle that sustains dysfunction if not addressed.
Key Causes of Female Erectile Dysfunction and Their Mechanisms
| Cause | Underlying Mechanism | Typical Impact on Arousal |
|---|---|---|
| Estrogen deficiency | Reduced lubrication and tissue elasticity | Vaginal dryness and discomfort |
| Low testosterone | Decreased sensory responsiveness | Reduced genital sensitivity |
| Cardiovascular disease | Impaired blood vessel dilation | Weak clitoral engorgement |
| Diabetes | Vascular damage and nerve impairment | Decreased sensitivity and delayed arousal |
| Antidepressants SSRIs | Altered neurotransmitter balance | Blunted arousal and delayed orgasm |
| Chronic stress | Elevated cortisol suppressing neural signaling | Reduced intensity of physical response |
| Smoking | Constricted blood vessels and low nitric oxide | Slower or weaker genital swelling |
This overview demonstrates that female erectile dysfunction is typically multifactorial. Accurate identification of the dominant cause allows clinicians to tailor treatment rather than applying a one size fits all approach.
Symptoms and Clinical Evaluation
Female erectile dysfunction is characterized by persistent physical difficulty achieving or maintaining adequate genital arousal. Temporary variation is normal and does not necessarily indicate a disorder. Diagnosis requires consistency, duration, and associated personal distress.
Common symptoms include reduced clitoral engorgement, insufficient vaginal lubrication, decreased genital sensitivity, difficulty sustaining physical excitement, and diminished sexual satisfaction specifically linked to impaired arousal rather than lack of desire.
Evaluation begins with a detailed medical and sexual history. Healthcare providers assess menstrual patterns, menopausal status, medication use, chronic illnesses, and stress levels. Because vascular health plays a central role, cardiovascular risk assessment is important.
Laboratory testing may include estrogen, testosterone, thyroid function, fasting glucose, and lipid profile. A pelvic examination can help evaluate tissue health and signs of hormonal deficiency. There is no single diagnostic test; clinicians identify patterns and rule out other causes before confirming female sexual arousal disorder.
Accurate diagnosis ensures that treatment is aligned with the underlying mechanism rather than applied generically.
Modern Treatment Options for Female Erectile Dysfunction
Effective treatment of female erectile dysfunction depends on identifying whether the primary driver is vascular, hormonal, neurological, psychological, or mixed. In 2026, management strategies are increasingly individualized, reflecting deeper clinical understanding of female sexual physiology.
Vascular Focused Treatment
Because genital engorgement relies on healthy blood vessel dilation, improving circulation is central when vascular insufficiency is involved. Nitric oxide activity enables blood vessels in clitoral tissue to expand during stimulation, allowing adequate swelling and sensitivity.
Pharmacological options developed to enhance genital blood flow may be considered for women who experience weak clitoral engorgement or difficulty maintaining physical arousal. One example is Female Viagra (Lovegra), formulated to support the vascular mechanism of female sexual response.
Both systemic and localized approaches are being used in clinical practice. Oral formulations influence circulation throughout the body, while topical solutions act directly on genital tissue. A detailed comparison of these methods, including mechanism and onset differences, is explained in Female Viagra Topical and Oral Solutions for Female Arousal in 2026. Proper medical screening is essential before starting any circulatory therapy.
Hormonal Therapy
When testing confirms estrogen deficiency, localized estrogen therapy may restore vaginal tissue elasticity and improve lubrication. In carefully selected cases, monitored androgen support may enhance sensitivity.
Hormone therapy must be personalized and supervised by a healthcare provider. It is most effective when a measurable imbalance contributes to symptoms rather than used indiscriminately.
Psychological and Behavioral Interventions
The brain plays a central role in sexual arousal. Anxiety, chronic stress, unresolved trauma, and relationship tension can suppress neural signaling even when vascular function is intact.
Sex therapy, cognitive behavioral therapy, and couples counseling may improve communication and reduce performance pressure. When physical and psychological factors coexist, integrated treatment tends to produce stronger and more sustainable improvement.
Lifestyle and Circulatory Support
Genital blood flow reflects overall cardiovascular health. Supporting vascular integrity strengthens the physiological basis of arousal.
Evidence based lifestyle strategies that may improve sexual responsiveness include
- Regular aerobic exercise to enhance endothelial function
- Smoking cessation to restore vascular dilation capacity
- Balanced nutrition supporting nitric oxide production
- Blood pressure, cholesterol, and glucose control
- Stress reduction practices to normalize cortisol levels
These interventions may not create immediate changes, but they reinforce long term circulatory health and nerve responsiveness.
Myths and Misconceptions
Despite increased awareness, several misconceptions persist.
One myth is that female erectile dysfunction is simply a normal part of aging. While hormonal changes increase risk, persistent arousal problems are not inevitable and should not be dismissed. Another misunderstanding is that the condition is purely psychological. Research clearly shows that vascular, hormonal, and neurological mechanisms are frequently involved. Ignoring biological factors may delay effective care. There is also a belief that medical treatment options for women are limited. In reality, advances in circulatory therapies, hormonal strategies, and localized formulations have expanded available solutions significantly.
Occasional difficulty becoming aroused does not automatically indicate dysfunction. Diagnosis requires persistence and associated distress.
Medical Disclaimer
This article is for informational purposes only and does not constitute medical advice. Always consult a qualified healthcare professional regarding any medical condition or treatment.
Author:
Dr. Cody R. Christensen
Frequently Asked Questions
Can women experience erectile dysfunction similar to men
Yes. Women have erectile tissue in the clitoris that depends on proper blood flow and nerve signaling, and impairment can reduce physical arousal.
What are the most common symptoms
Typical symptoms include reduced clitoral swelling, insufficient lubrication, decreased genital sensitivity, and difficulty maintaining physical excitement.
Is female erectile dysfunction permanent
In many cases it is treatable. Improvement often occurs once vascular, hormonal, or psychological causes are properly addressed.
Does menopause automatically cause arousal problems
Menopause increases the likelihood due to estrogen decline, but not every woman develops dysfunction and effective therapies are available.
When should medical evaluation be considered
If symptoms persist for several months, cause emotional distress, or affect relationship satisfaction, professional assessment is recommended.
Resources
- MedlinePlus – explaining female sexual dysfunction, underlying medical causes, and evidence-based treatment approaches.
- ACOG – women’s sexual health concerns, including arousal problems and when to seek medical care.
- NHS – reduced sexual desire and arousal difficulties, with guidance on causes and available treatments.
